Overview – Eating behaviour
This A level psychology topic looks at the psychology and biology underlying eating behaviour, such as different food preferences and the psychology of eating disorders:
- Explanations of food preferences (including evolutionary and learning explanations)
- The biological mechanisms involved in the control of eating (including the role of the hypothalamus and the hormones ghrelin and leptin)
- Explanations of anorexia nervosa (including biological explanations such as genetics and neural factors, as well as psychological explanations such as family systems theory, social learning theory, and cognitive explanations)
- Explanations of obesity (including biological explanations such as genetics and neural factors, as well as psychological explanations such as the boundary model and restraint theory)
Explanations of food preferences
Evolutionary explanations
Evolution is the process by which species adapt to their environment. Over many many years, random mutations in genes that are advantageous to the animal become more widespread among the species.
In the case of food, evolution would mean genes that help humans identify and eat healthy, safe, and nutritious food will become more common. If you had genes that resulted in a preference for nutritious and commonly-found foods, for example, you would be less likely to starve and more likely to remain healthy and pass on those genes. In contrast, if you had genes that meant you really liked the taste of deadly mushrooms, you probably wouldn’t live long enough to reproduce and pass on those genes.
 Evolution can explain human preferences for different foods. For example, sweet foods are often high in energy, which can also be stored as fat to reduce the chance of starvation. In contrast, poisons often have a bitter taste, which may explain why humans generally prefer sweet foods to bitter ones – it’s genetic.
Evolution can explain human preferences for different foods. For example, sweet foods are often high in energy, which can also be stored as fat to reduce the chance of starvation. In contrast, poisons often have a bitter taste, which may explain why humans generally prefer sweet foods to bitter ones – it’s genetic.
Neophobia
Neophobia is an innate dislike of foods we haven’t tried before. This makes sense from an evolutionary perspective as unfamiliar foods could potentially be poisonous or unhealthy. You’re more likely to survive if you stick with familiar foods as you already know they’re safe.
We overcome neophobia via learning. In a study of young children, Birch et al (1987) found that preference for new foods increased over time with repeated exposure to those foods.
Taste aversion
Taste aversion is when a person develops a dislike for a certain food after becoming ill from it. For example, you eat yoghurt, get food poisoning, and from then on even the thought of eating yoghurt again makes you feel sick.
Although kind of like classical conditioning, taste aversion doesn’t work in quite the same way because the time between eating the food and getting ill is often quite long. Instead, the more accurate description is biological preparedness (Seligman (1971)), which is the idea that humans are biologically hard-wired to learn certain kinds of associations very easily. This would make sense from an evolutionary perspective: If certain foods are dangerous, it would be advantageous to learn this as quickly as possible because the next time you eat that food you might get ill again or die.
AO3 evaluation points: Evolutionary explanations of food preferences
- Evidence supporting evolutionary explanations: Several studies (e.g. Desor et al (1973), Steiner (1979), and Rosenstein and Oster (1988)) have analysed the facial expressions and behaviours of babies after feeding them bitter- and sweet-tasting foods, finding that babies like sweet tastes and dislike bitter ones. The fact that the babies have these food preferences from such a young age suggests they are innate, supporting evolutionary explanations of food preferences.
- Evolved for survival in a different era: Human food preferences would have evolved in a time when food was scarce, but these food preferences are somewhat maladaptive in the modern era where food is plentiful. For example, early humans would feast on high energy and fattening foods on the rare occasions when they were available in order to prevent starvation. However, such foods are now easily available and so these evolutionary preferences can lead to obesity in the modern era.
- Other factors: Although evolution plays a role in shaping food preferences, other factors influence food preferences too. For example, social influences can override evolutionarily-programmed neophobia, such as a mother feeding her child new foods. Cultural influences are also important. For example, a person may have genetics that predispose them towards liking the taste of Marmite, but if they are not raised in a culture that has Marmite then they may never develop this taste.
The role of learning
In addition to genetic/evolutionary factors, humans also learn food preferences from social influences and their culture.
Social influences
There are several ways social influences affect food preferences.
Firstly, what a child’s mother eats during development affects the child’s food preferences. In the womb, foods (and flavours) the mother eats are fed to the baby via the amniotic fluid. After birth, foods and flavours are transmitted from the mother to the baby via breast milk. This contributes towards a preference for the same foods as the mother.
 Secondly, social learning affects food preferences. Children observe what parents and other role models eat, which they then imitate. This helps reduce neophobia, encouraging the child to eat a wider range of foods.
Secondly, social learning affects food preferences. Children observe what parents and other role models eat, which they then imitate. This helps reduce neophobia, encouraging the child to eat a wider range of foods.
Thirdly, operant conditioning also contributes to food preferences. If you enjoy eating a certain food, then that enjoyment serves as positive reinforcement, which increases the chances of you eating it again. However, research suggests that operant conditioning doesn’t really work to create food preferences. For example, if parents try to teach their children to like certain foods (e.g. vegetables) through rewards (e.g. praise for eating vegetables), it may actually decrease preference for those foods.
Cultural influences
Different cultures have different eating behaviours and these cultural influences affect food preferences. For example, some religious cultures (e.g. Islam and Judaism) forbid eating pork, whereas others forbid eating beef (e.g. Hinduism). Different cultures also have different local cuisines (e.g. eating snails in France (escargots), raw octopus in Korea (san-nakji)), which affect food preferences.
AO3 evaluation points: Learning explanations of food preferences
- Evidence supporting learning explanations: Mennella et al (2005) found that genetics primarily determine food preferences in children (e.g. liking sweet tastes and disliking bitter ones) but by adulthood environmental factors are far more important, supporting learning explanations of food preferences.
- Changing influence of culture on food preferences: Advances in transportation (e.g. shipping) and technology (e.g. refrigeration) mean people have access to, and develop preferences for, foods they otherwise would not have. For example, avocados can’t be grown in the UK, which in the past would mean people living in the UK would not develop a taste for avocados. These economic and technological changes have reduced the impact of local culture on food preferences, making food preferences more global.
- Practical applications: Understanding the social and cultural influences of food preferences has useful applications. For example, if mothers transmit food preferences to their children in the womb, it makes sense for mothers to eat healthily during pregnancy to avoid passing on a taste for unhealthy foods to their children. In the case of culture, health agencies can tailor dietary advice to the culture they operate in.
Neural and hormonal mechanisms
Neural and hormonal mechanisms control eating behaviour biologically, making you feel hungry or full. The main neural mechanism is activity in the hypothalamus region of the brain, and the main hormones responsible for hunger and satiety are ghrelin and leptin.
Neural mechanisms
Hypothalamus
The hypothalamus is the main section of the brain responsible for maintaining homeostasis (i.e. stability and normal functioning) within the body. It controls things like body temperature, sleep, and hunger.
In the case of hunger, there are two sections of the hypothalamus that have opposite effects:
- Lateral hypothalamus: Responsible for making you feel hungry and start eating.
- Ventromedial hypothalamus: Responsible for making you feel full (satiety) and stop eating.
The process is as follows: When blood sugar (glucose) is low, the liver sends signals to the lateral hypothalamus. This causes neurons to fire that make you feel hungry and start eating. Then, when you eat, glucose is released into the blood, which is detected by the ventromedial hypothalamus. This causes neurons to fire that make you feel satiated (full).
Hormones
Ghrelin
Ghrelin is a hormone that makes you feel hungry. It is secreted by the stomach into the bloodstream, which is detected by the hypothalamus, creating the sensation of hunger. When you eat food, the stomach stops releasing ghrelin, which stops you feeling hungry. After the meal is eaten, ghrelin levels (and hunger) progressively increase until the next time you eat.
Leptin
Leptin is a hormone that makes you feel full. It is secreted by fat cells into the bloodstream, which signals to the hypothalamus that energy storage (fat deposits) is high and so you don’t need to eat. If you don’t eat for a while, the body uses these fat deposits for energy, and so those fat cells no longer exist to produce leptin. This reduction in leptin makes you feel hungry.
Explanations of anorexia
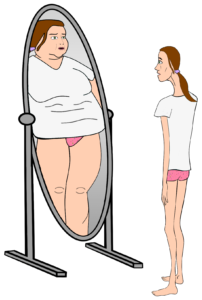 Anorexia nervosa is an eating disorder characterised by an obsession with losing weight, body image distortion, restriction of food consumption, and low bodyweight. Estimates vary, but anorexia affects roughly 1% of the population, of which 85% are female.
Anorexia nervosa is an eating disorder characterised by an obsession with losing weight, body image distortion, restriction of food consumption, and low bodyweight. Estimates vary, but anorexia affects roughly 1% of the population, of which 85% are female.
The syllabus looks at biological and psychological explanations of anorexia.
Biological explanations
Biological explanations of anorexia look at the role of genetics and neural factors (such as brain structures and neurotransmitter activity).
Genetics
The genetic explanation of anorexia looks at hereditary factors – i.e. genes inherited from parents – that contribute to the development of anorexia.
As always, twin studies are a useful way to work out the extent to which a condition is genetically determined. If identical twins are more likely to both suffer from anorexia than both non-identical twins are, this would suggest anorexia is (at least partly) determined by genetics. Twin studies of anorexia include:
- Holland et al (1988) found a concordance rate for anorexia of 56% for identical twins and 5% for non-identical twins.
- Kortegaard et al (2001) found a concordance rate for anorexia of 18% for identical twins and 7% for non-identical twins.
- Bulik et al (2006) estimate the heritability of anorexia is 56% based on analysis of 31,406 pairs of Swedish twins.
Despite variations in estimates, the fact that identical twins are more likely to both suffer from anorexia than non-identical twins suggests there is a genetic component to the disorder.
The role of genetics is further supported by gene association studies (e.g. Wang et al (2011) and Scott-Van Zeeland et al (2014)), which compare DNA profiles of anorexia sufferers with non-anorexic controls. These studies have found various genes to be correlated with anorexia, such as OPRD1, HTR1D, and EPHX2.
AO3 evaluation points: Genetic explanations of anorexia
Strengths of genetic explanations:
- Evidence supporting genetic explanations: See studies above (don’t worry, you don’t have to remember all of them – they’re just examples).
Weaknesses of genetic explanations:
- Other factors: Although there is strong evidence for a genetic component to anorexia, the evidence also suggests that other factors are important too. For example, if anorexia was entirely explained by genetics, concordance rates among identical twins would be 100% – but they’re not. The fact that even the highest figures estimate anorexia to be 56% heritable leaves 44% to be accounted for by factors other than genetics.
- Limitations of genetic explanations: Anorexia was practically unheard of before 1950 but since then rates of anorexia have increased significantly. This change is far too quick to be explained by genetics because only a few generations have passed since then. This suggests factors other than genetics (e.g. social learning theory) are contributing to the rise in anorexia diagnoses.
- Methodological concerns with twin studies: Twin studies typically assume that twins have identical upbringings and so any differences in concordance rates between identical and non-identical twins must be explained entirely by genetics. However, environmental factors may play a more important role than studies assume. For example, looking identical probably makes parents treat identical twins more similarly than they would non-identical twins. This may explain (at least partly) why identical twins have higher concordance rates for anorexia than non-identical twins, which would mean the role of genetics is exaggerated.
Neural factors
Neural explanations of anorexia look at differences in the brain structures and neurochemistry of people with anorexia.
Some research suggests that people with anorexia have reduced blood flow in the lateral hypothalamus (the part of the brain associated with hunger), but it is unclear whether this is a cause or an effect of anorexia. More recently, researchers (e.g. Nunn et al (2011)) have proposed that damage to the insula cortex of the brain is a key cause of anorexia.
In addition to physical brain structures, neural explanations of anorexia also focus on the role of neurotransmitters. For example, several studies have found correlations between serotonin activity and anorexia, although the exact relationship is unclear. One hypothesis proposed by Kaye et al (2009) is that anorexic patients naturally have elevated serotonin activity, which causes them anxiety. Starvation reduces serotonin levels (food is needed to produce serotonin), which reduces this anxiety and reinforces anorexic behaviour. Research (e.g. Bailer et al (2013)) also suggests over-production of the neurotransmitter dopamine may contribute to anorexia.
AO3 evaluation points: Neural explanations of anorexia
Strengths of neural explanations:
- Evidence supporting neural explanations: See studies above (again, you don’t have to remember all of them – they’re just examples).
- Practical applications: If neural explanations of anorexia are identified, this could lead to effective ways to treat the disorder. For example, some studies suggest SSRIs can improve anorexia outcomes by altering neurotransmitter activity (although other studies dispute this).
Weaknesses of neural explanations:
- Conflicting evidence: Much of the research linking neurotransmitter activity and anorexia is contradictory. For example, a review by Kontis and Theochari (2012) reports how different studies have suggested anorexia is linked with normal, increased, and decreased dopamine activity.
- Correlation vs. causation: Even if certain abnormalities in brain structures (or neurotransmitter activity) are correlated with anorexia, this doesn’t automatically prove that this is the cause of anorexia. For example, reduced blood flow in the lateral hypothalamus could be an effect of starvation rather than a cause of anorexia.
Psychological explanations
There are several psychological explanations of anorexia, including family systems theory, social learning theory, and cognitive explanations.
Family systems theory
Minuchin et al (1978) proposed the family systems theory of anorexia, which is a psychodynamic theory that explains anorexia as a result of family dysfunction. According to the family systems theory, the families of anorexic patients often share four key features:
- Enmeshment: The family members have no individual identity or independence but instead blur into one single unit. For example, they are very involved in each other’s business, spend all their time together, and nobody has any unique role within the family.
- Overprotective: The family is very controlling and overprotective, which makes it more difficult for members to break free from the enmeshment and develop their own identity.
- Conflict avoidance: The family ignores or suppresses conflict. For example, they won’t discuss obvious problems.
- Rigidity: The family does not like change and tries to keep things as they are.
This dysfunctional family style can contribute to anorexia in various ways. For example, becoming anorexic may be a way to reduce conflict by distracting the family members from other problems. For example, a child who fears their parents will split up due to constant arguing may become anorexic in order to shift the parents’ attention away from those arguments, keeping the family together.
A related explanation (e.g. Bruch (1978)) is that anorexia is a way for people to assert autonomy and control. For example, refusing to eat might be a way for a family member to assert their individuality and free will against their overprotective and enmeshed family.
AO3 evaluation points: Family systems theory explanation of anorexia
Strengths of family systems theory:
- Evidence supporting family systems theory: In Minuchin et al (1978), the researchers got 11 families of anorexic patients and 34 control families to complete a group task. The researchers observed greater levels of enmeshment, overprotectiveness, conflict avoidance, and rigidity among the families of anorexic patients, providing support for all four elements of the family systems model.
- Practical applications: Some studies have found family systems therapy to be an effective treatment for anorexia. For example, Robin et al (1999) randomly assigned 37 anorexic patients to receive either family systems therapy or individual therapy. Although both treatments were found to be effective, the family systems therapy group saw greater weight gains and a faster return to health. However, a review of several trials by Fisher et al (2019) found the evidence was insufficient to say family-based treatments are more effective than other approaches.
Weaknesses of family systems theory:
- Conflicting evidence: A review of 17 studies by Viesel and Allan (2014) found that anorexia and family dysfunction were correlated. However, the researchers did not find evidence for a specific pattern of family dysfunction (e.g. enmeshment), weakening support for Minuchin et al’s family systems model.
- Other factors: Even if family dysfunction does contribute to anorexia, it’s unlikely to be the sole cause. For example, many anorexic patients develop anorexia in adulthood – long after leaving their families – which suggests that other factors (e.g. biology or social learning) contribute to the disorder as well.
- Correlation vs. causation: Even if certain types of family dysfunction (e.g. enmeshment) are correlated with anorexia, this does not automatically prove this is what causes anorexia. For example, a child developing anorexia could cause a previously normal family to become more enmeshed, rather than the other way round.
Social learning theory
Social learning theory (see the approaches page for more details) explains anorexia as learned behaviour from observation and imitation of role models.
According to social learning theory, people imitate the behaviours of role models they identify with. These behaviours may be enforced vicariously, i.e. by seeing the role model be praised and rewarded for that behaviour. This can be applied to anorexia:
- Modelling: A person who the anorexic patient either likes or wants to be like. For example, an older sister or a celebrity who is thin.
- Vicarious reinforcement: The anorexic patient observes the role model being rewarded and praised for being thin. For example, the slim sister is complimented on her weight loss, or the slim celebrity has lots of followers on social media. These rewards create a motivation to imitate their behaviour and restrict eating.
The syllabus mentions social learning theory specifically, but other learning approaches (operant conditioning) may also reinforce anorexic behaviour. For example, when the anorexic patient starts imitating the behaviour themself, they may receive compliments for being slim (positive reinforcement) or people may stop criticising them for being overweight (negative reinforcement).
 The media plays an important part in social learning explanations of anorexia. For example, singers, actresses, and models in magazines and social media are often depicted as slim, and slimness is depicted as desirable – especially in Western cultures. The praise these role models receive in the media provides further vicarious reinforcement of losing weight, which may lead to anorexia.
The media plays an important part in social learning explanations of anorexia. For example, singers, actresses, and models in magazines and social media are often depicted as slim, and slimness is depicted as desirable – especially in Western cultures. The praise these role models receive in the media provides further vicarious reinforcement of losing weight, which may lead to anorexia.
AO3 evaluation points: Social learning explanations of anorexia
Strengths of social learning explanations:
- Evidence supporting social learning explanations: For example, Dittmar et al (2006) showed 162 girls (aged 5-8) either Barbie dolls, Emme dolls (a US size 16), or no dolls and then got them to complete a body image assessment. The girls shown the Barbie dolls had lower body esteem and a greater desire to be thin than the other two groups, supporting the explanation that role models in the media and culture may contribute to anorexia. Another study, Garner et al (1980), looked at data from Playboy magazine models and Miss America contests over the years and found a trend towards a thinner standard of beauty over time, further supporting the social learning explanation.
- Explanatory power: Social learning theory is able to explain aspects of anorexia that other explanations aren’t. For example, anorexia has increased significantly since 1950 – far quicker than can be explained via changes in genetics. But social learning theory can explain this by pointing to things like growing emphasis on thinness in the media and culture during this time.
- Practical applications: If the social learning theory explanation of anorexia is correct, then it can be used to develop ways to treat and prevent anorexia. For example, the media could promote desirable heavier women as much as it does thinner women.
Weaknesses of social learning explanations:
- Other factors: Even if social learning and media influence contribute to anorexia, it’s unlikely this is the sole cause. For example, all women in Western countries are exposed to the same amount of media influence (more or less), and yet only some of these women develop anorexia. This suggests that other factors (e.g. biology) play a role too.
Cognitive explanations
Cognitive explanations of anorexia explain the disorder as a result of abnormal cognitions. These abnormal cognitions take the form of distortions and irrational beliefs:
- Distortions: Inaccurate perceptions of body image.
- E.g. The person sees their body as fat and overweight when actually it is skinny and underweight.
- Irrational beliefs: Incorrect, maladaptive, and exaggerated thoughts about eating food and gaining weight.
- E.g. “If I eat one crisp, I will get fat” or “If I can’t control my weight, I’m worthless”.
AO3 evaluation points: Cognitive explanations of anorexia
Strengths of cognitive explanations:
- Evidence supporting cognitive explanations: Several studies have found anorexic patients to have distorted body image compared to controls. For example, Williamson et al (1993) used silhouette pictures to evaluate 37 anorexic patients’ current and ideal body images. Compared to the control group, the anorexic patients’ estimation of their current body size was larger and their ideal body image was thinner, supporting the role of cognitive distortions in anorexia. Studies also support the presence of irrational beliefs in anorexia. For example, Steinglass et al (2007) investigated the main belief that prevented anorexic patients from eating. Of 25 anorexic patients surveyed, 68% had a main fear of gaining weight and 20% were categorised as delusional, supporting the role of irrational beliefs in anorexia.
- Practical applications: Cognitive explanations of anorexia have been used to develop effective treatments for the disorder. For example, Grave et al (2014) used cognitive behavioural therapy with 26 anorexia patients, which resulted in improvements in weight and anorexia symptoms that were still maintained at 12-month follow up.
Weaknesses of cognitive explanations:
- Conflicting evidence: In a study comparing 30 anorexic women with 137 controls, Cornelissen et al (2013) found no significant difference in body image estimates, which contradicts Williamson et al (1993) and weakens support for the role of cognitive distortions in anorexia.
- Other factors: Even if cognitive factors play a role in anorexia, it’s clear other factors are important too. For example, twin studies provide strong evidence for a genetic component to anorexia. It’s likely that many factors – cognitive, social, biological – combine to cause anorexia.
- Correlation vs. causation: Although cognitive distortions and irrational beliefs are correlated with anorexia, they may not be the cause of anorexia. For example, cognitive distortions may be a symptom of anorexia rather than the cause.
Explanations of obesity
 Obesity is a physical condition characterised by excess body fat, which may cause other health problems such as heart disease and diabetes. It is a leading cause of preventable death in many countries, including the UK. In the UK, around 30% of the population is classified as obese.
Obesity is a physical condition characterised by excess body fat, which may cause other health problems such as heart disease and diabetes. It is a leading cause of preventable death in many countries, including the UK. In the UK, around 30% of the population is classified as obese.
The syllabus looks at biological and psychological explanations of obesity.
Biological explanations
Biological explanations of obesity look at the role of genetics and neural factors (such as brain structures and neurotransmitter activity).
Genetics
The genetic explanation of obesity looks at hereditary factors – i.e. genes inherited from mother and father – that make someone more or less likely to become obese.
Again, as always, family and twin studies are a useful way to work out the influence of genetics on obesity. Some examples include:
- Stunkard et al (1990) compared concordance rates of obesity among identical twins raised together and identical twins raised apart (and also non-identical twins raised together and apart). Male and female identical twins raised together had concordance rates of 74% and 69% respectively, whereas male and female twins raised apart had concordance rates of 70% and 66% respectively. The similarity between these two sets of figures suggests the different environments had little impact on obesity rates compared to genetics.
- Nan et al (2012) estimate the concordance rate of obesity among identical twins is 61-80%.
- Chaput et al (2014) looked at obesity among families, estimating that obesity is 35-60% heritable.
In addition to these family studies, genome association studies compare the genetic profiles of obese individuals with non-obese controls to identify genes that may contribute to obesity. For example, several studies (e.g. Fall and Ingelsson (2012), Frayling et al (2007), and Hinney et al (2007)) have found the FTO gene to be correlated with obesity. However, there is no single obesity gene – many genes appear to combine to increase or decrease a person’s risk for obesity.
AO3 evaluation points: Genetic explanations of obesity
Strengths of genetic explanations:
- Evidence supporting genetic explanations: See studies above (again, you don’t need to remember them all – they’re just examples).
- Practical applications: An understanding of the genetic basis for obesity could lead to effective treatments for the disorder. For example, genetics may mean certain foods may be particularly fattening for some individuals, which could inform diet plans that help them lose weight more effectively.
Weaknesses of genetic explanations:
- Other factors: Although there is evidence of a genetic component to obesity, there is clearly more to the story than just genes. For example, the concordance rates of obesity among identical twins is far less than 100%, which suggests other factors (e.g. psychological) play a role too.
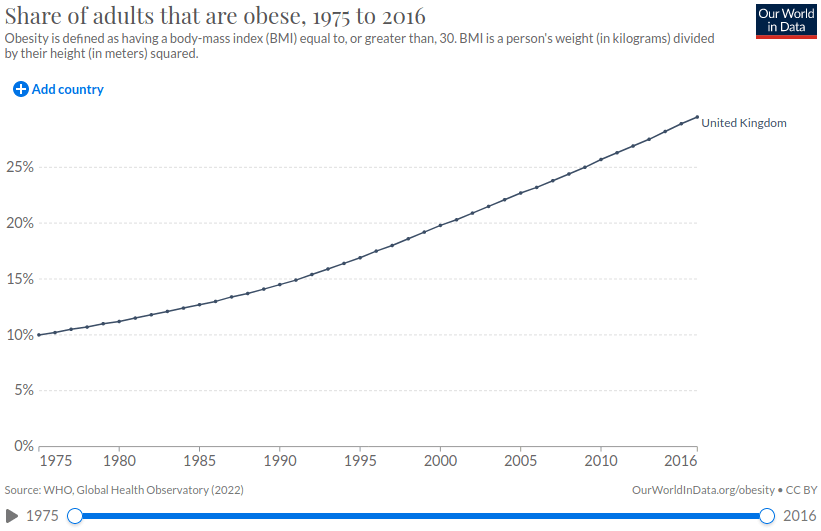
- Limitations of genetic explanations: Obesity has increased dramatically over the last few decades (see chart below). This change has happened far too quickly to be explained by genetics as only a few generations have passed during this time. This further suggests that other factors (e.g. changing dietary habits) play an important role in explaining obesity.
Neural factors
Neural explanations of obesity focus on the neural mechanisms that control eating behaviour as well as the role of neurotransmitters such as serotonin and dopamine.
As described above, the hypothalamus plays a key role in eating behaviour. Some neural explanations say that damage to the ventromedial hypothalamus – the area of the brain responsible for making you feel full – can cause obesity. Other explanations look at the role of leptin – the hormone that makes you feel full – saying that obesity can be caused by neurons that don’t respond properly to this hormone.
Neurotransmitters are also implicated in obesity. For example, Wang et al (2001) and Volkow et al (2008) have used brain scans to measure dopamine receptor activity in obese individuals and controls, with both studies finding that obese individuals have reduced dopamine receptor activity. Dopamine is associated with pleasure and reward and so the associated hypothesis is that obese people overeat to get the same pleasure and reward response as a non-obese person would get from eating less food. This is a similar mechanism to other addictions, such as smoking or drugs.
Other studies (e.g. Hodge et al (2012) and Vickers et al (1999)) suggest lower serotonin levels are also correlated with obesity.
AO3 evaluation points: Neural explanations of obesity
Strengths of neural explanations:
- Evidence supporting neural explanations: See studies above.
- Practical applications: Identifying the neural factors that cause obesity could lead to new ways to treat the disorder. For example, some studies (e.g. Heymsfield et al (1999)) suggest leptin injections may be a successful treatment for obesity in some people. Other treatments could address dopamine and serotonin deficiencies.
Weaknesses of neural explanations:
- Conflicting evidence: For each neural explanation of obesity, there are often several studies that contradict it. For example, a meta-analysis of 33 studies by Benton and Young (2016) found lower dopamine receptor activity is not correlated with obesity, contradicting the findings of Wang et al (2001) and Volkow et al (2008) described above.
- Other factors: Although there is some evidence supporting neural explanations obesity, it’s likely other factors, such as genetics, play a larger role in explaining the disorder.
- Correlation vs. causation: Even if certain neurological patterns (e.g. low dopamine sensitivity) are correlated with obesity, this doesn’t prove these neurological patterns cause obesity. For example, obesity could be caused entirely by psychological factors, with low dopamine sensitivity simply being a symptom of the disorder.
Psychological explanations
There are several psychological explanations of obesity, including the boundary model and restraint theory. This section also looks at psychological explanations of the success and failure of dieting.
Boundary model
Herman and Polivy (1984) proposed the boundary model. According to this model, people have biologically-set boundaries of food intake. If food falls below a certain minimum level, the person feels the aversive (unpleasant) feeling of hunger that motivates them to eat. At the other end, eating too much food exceeds the maximum level, which causes the aversive feeling of being too full. These levels are primarily determined by biology.

The range in the middle is the zone of biological indifference, where a person’s biology is satisfied. And so, within this zone, psychological factors are more important than biological ones in determining whether a person eats. In other words, a person who consumes food within this zone does not do so for biological reasons (i.e. to avoid starvation), but for psychological reasons.
Restraint theory
According to restraint theory, trying to eat less can paradoxically make a person eat more and become obese.
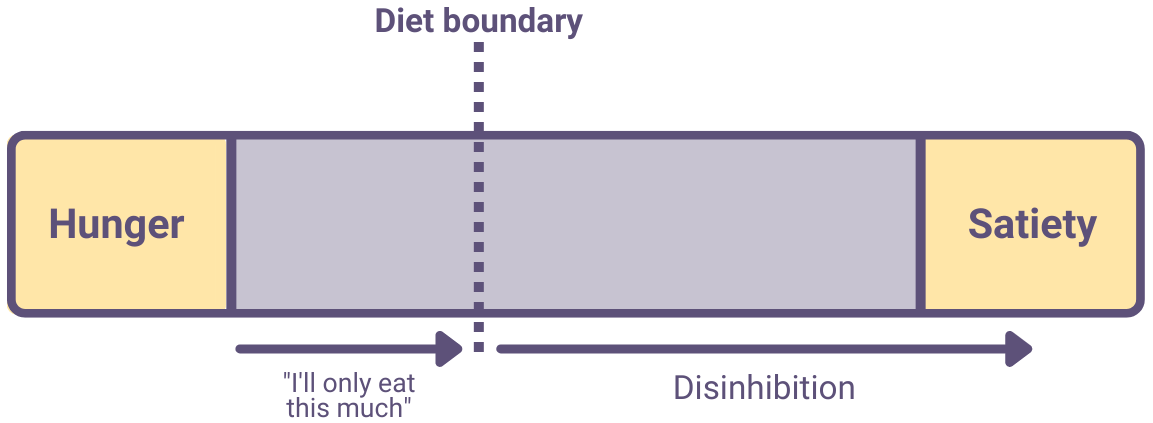
One explanation of this is as follows:
- A restrained eater will set a diet boundary. This is a self-imposed cognitive limit after which they won’t eat any more.
- Setting this boundary causes the restrained eater to spend a lot of time thinking about food – more so than if they hadn’t set a diet boundary. Also, the diet boundary may be unrealistically low, causing constant hunger and low mood.
- When the person crosses their diet boundary (as often happens), their eating may become disinhibited: They give up trying to control their eating and keep eating until they’re full (or beyond).
- Disinhibited eating causes obesity.
AO3 evaluation points: Restraint theory explanation of obesity
Strengths of restraint theory:
- Evidence supporting restraint theory: For example, Herman and Mack (1975) categorised 45 normal-weight women as restrained (i.e. dieting) or unrestrained (i.e. non-dieting) eaters. The women were randomly separated into groups given either one glass of milkshake, two glasses of milkshake, or nothing. After the milkshakes, they were then given unlimited ice cream to eat. The researchers found that the unrestrained eaters ate less ice cream the more milkshakes they’d had previously, which is to be expected as presumably they were already full. However, the restrained eaters actually ate more ice cream the more milkshakes they’d had previously, suggesting they had become disinhibited. Further studies supporting restraint theory include Ruderman and Wilson (1979) and Wardle and Beales (1988).
- Practical applications: It seems obvious that dieting is an effective way to lose weight, but restraint theory suggests the opposite might actually be true. Knowing this could lead to more effective ways to reduce obesity. For example, Bergh et al (2009) describes how training people to eat more slowly (rather than dieting) might be an effective treatment for obesity.
Weaknesses of restraint theory:
- Conflicting evidence: There are many examples of people who have successfully lost weight via dieting, which weakens support for restraint theory. For example, in a longitudinal study of 163 women, Savage et al (2009) found that restrained eating and dieting were correlated with weight loss, not weight gain. This directly contradicts the predictions of restraint theory and challenges its validity.
- Correlation vs. causation: Being a restrained eater may simply be correlated with obesity, rather than a cause of obesity. For example, people who are naturally prone to obesity may be more likely to set themselves dietary restrictions, rather than these dietary restrictions causing them to become obese.
Explanations of the success/failure of dieting
A diet is successful if the dieter loses the desired amount of weight and keeps it off for the long-term. There are many factors that contribute to the success or failure of dieting.
Factors that increase the chance of success include:
- Realistic expectations: Dieters are more likely to succeed if they follow a sustainable diet and steadily lose weight over a period of months and years, setting realistic short- and long-term goals.
- Incentives and motivation: Dieters may reward themselves for achieving weight loss goals. For example, a dieter may buy new clothes to fit their slimmer physique. This works as a form of operant conditioning, reinforcing and motivating weight loss.
- Social support: Having support from family and friends makes a diet more likely to succeed. For example, Wing and Jeffery (1999) randomly assigned 166 participants to receive either a standard 4-month weight loss program or a standard 4-month weight loss program + social support. At follow up 6 months later, 66% of participants in the social support group had maintained their weight loss compared to just 24% in the group without social support.
- Relapse prevention strategies: Many dieters see dieting as a temporary measure after which they can return to their old eating habits. This results in a demotivating cycle of regaining lost weight and then dieting again (yo-yo dieting). Dieters who have strategies to avoid going back to their previous eating behaviours and maintain a stable food intake are more likely to succeed.
Factors that increase the chance of failure include:
- Overly-restrictive diets: Dieters often try to follow diets that are too strict, such as limiting calories to under 1000 per day. This is unsustainable and when the dieter exceeds this limit they may lose motivation and indulge in disinhibited eating (in line with the predictions of restraint theory).
- Unrealistic expectations: Dieters often expect to lose a lot of weight in a matter of weeks or months. However, obese people typically gained weight progressively over many years and so it is unrealistic to expect to reverse this in a short time period. If the dieter does not have realistic expectations, they may lose motivation and abandon the diet.
In addition to these psychological factors, other factors (e.g. genetics) affect the success or failure of dieting.
AO3 evaluation points: Explanations of the success/failure of dieting
- Individual differences: Although there are general ways to increase the chance of diet success, the best approach is likely to vary from person to person. For example, restrained eaters are unlikely to successfully lose weight via calorie restriction because this is likely to result in disinhibited eating. Unrestrained eaters, in contrast, are likely to have more success with calorie restriction.
- Practical applications: Understanding the factors that increase the likelihood of diet success could lead to more effective ways to treat obesity. For example, providing social support in addition to a realistic diet plan is likely to increase the chance of successful and sustainable weight loss.
- Gender bias: The majority of research into dieting is done on females, and so the conclusions drawn from this research may not be valid in males.
<<<Relationships
or:
<<<Gender
or:
<<<Cognition and development
Aggression>>>
or:
Forensic psychology>>>
or: