Overview – Stress
Stress is the body’s response when an individual feels they are unable to cope with a situation or challenge. This A level psychology topic looks at the following aspects of stress:e
- The physiology of stress (including general adaptation syndrome, the hypothalamic-pituitary-adrenal system, and the sympathomedullary pathway)
- The role of stress in illness (including immunosuppression and the role of stress in cardiovascular disorders)
- Sources of stress (including life changes, daily hassles, and workplace stress)
- Measuring stress (including self-report measures such as the social readjustment ratings scale and the hassles and uplifts scale, as well as physiological measures such as skin conductance response)
- Individual differences in stress (including personality types, hardiness, and gender differences in coping with stress)
- Ways of managing stress (including drug therapy, stress inoculation therapy, biofeedback, and social support)
The physiology of stress
 We have all experienced and know what stress is. But the precise psychological understanding of stress is when an individual feels (rightly or wrongly) that they are not able to cope with the demands of a situation. For example, if you feel like you don’t know enough to pass your psychology A level exam, this will cause you stress.
We have all experienced and know what stress is. But the precise psychological understanding of stress is when an individual feels (rightly or wrongly) that they are not able to cope with the demands of a situation. For example, if you feel like you don’t know enough to pass your psychology A level exam, this will cause you stress.
The physiology of stress is the study of the biological processes underlying stress. Stressors (causes of stress) prompt a physiological response, that was first described as general adaptation syndrome by Hans Selye. Later explanations break this response down into the following biological systems:
- The sympathomedullary pathway (acute, short-term stress)
- The hypothalamic-pituitary-adrenal system (chronic, long-term stress)
General adaptation syndrome
Selye (1936) conducted experiments where rats were exposed to various stressors such as extreme cold, forced exercise, and sub-lethal doses of drugs. He observed a common physiological sequence in response to these stressors:
- Alarm reaction: The hypothalamus sends a signal to the sympathetic nervous system to release adrenaline and noradrenaline (see fight or flight in the biopsychology page for more details) in order to overcome the stressor.
- Resistance: If the stressor hasn’t gone away, the body keeps pumping out adrenaline and noradrenaline, but levels decline. The body increases the level of cortisol in the blood to provide energy to cope with the stress. At this stage, the body is using resources at a harmful rate that cannot be maintained.
- Exhaustion: If the stressor still hasn’t gone away, the body starts running out of resources to maintain constantly elevated levels of stress hormones and sympathetic nervous system activity. This can manifest as physical symptoms such as low blood sugar, high blood pressure, immunosuppression, and stress-related illnesses such as heart disease.
The fact that this same general sequence was observed irrespective of the specific stressor led Selye to characterise this 3-part stress response as general adaptation syndrome.
AO3 evaluation points: General adaptation syndrome
Strengths of general adaptation syndrome:
- Supporting evidence: Selye’s (1936) experiments on rats demonstrated the same physiological sequence in response to completely different stressors. This supports general adaptation syndrome as a single and complete explanation of stress.
Weaknesses of general adaptation syndrome:
- Conflicting evidence: Mason (1971) conducted experiments similar to Selye’s (1936) but on monkeys instead of rats. In these experiments, rather than exhibiting the same physiological response to the different stressors, the monkeys’ physiological responses differed depending on the stressor. For example, exposure to extreme cold appeared to increase levels of cortisol whereas exposure to extreme heat decreased cortisol levels. This suggests that the explanation of stress as general adaptation is not accurate and is instead specific to different stressors.
- Methodological concerns: As Selye’s (1936) physiological explanation of stress was derived from experiments on rats, general adaptation syndrome may not be valid when explaining the physiological process of stress in human beings.
The sympathomedullary pathway
The sympathomedullary pathway is associated with acute (short-term) stress.
When a person encounters a stressor, the following sequence takes place:
- The hypothalamus sends a signal to the sympathetic part of the autonomic nervous system
- This signal triggers the adrenal medulla of the adrenal glands to release the hormones adrenaline and noradrenaline
- These hormones increase bodily activities to prepare to deal with the stressor. For example, heart rate and breathing are increased to improve blood flow and oxygenation, and bodily systems that are not essential for dealing with the stressor (e.g. digestion) are decreased.
Note: This is basically the fight or flight response from the biopsychology topic.
Once the stressor has gone away, the parasympathetic part of the autonomic nervous system reduces bodily activity and switches from fight or flight back to rest and digest.
However, if the stressor remains for an extended time period, the long-term stress response of the hypothalamic-pituitary-adrenal system takes over.
The hypothalamic-pituitary-adrenal system
The hypothalamic-pituitary-adrenal system is associated with chronic (long-term) stress.
The short-term sympathomedullary response cannot be maintained for extended periods because it consumes too many bodily resources. So, if a stressor remains, the following sequence takes place:
- The hypothalamus starts releasing corticotropin-releasing hormone (CRH)
- CRH tells the pituitary gland to start releasing adrenocorticotropic hormone (ACTH)
- ACTH tells the adrenal cortex of the adrenal glands to release cortisol, which provides energy.
Cortisol
Cortisol is a glucocorticoid hormone that increases blood sugar by converting protein to glucose. This increased blood sugar provides energy to replace the energy lost during the sympathomedullary response and help overcome the stressor.
However, cortisol has negative effects on the body – especially over the long term. For example, excessively high cortisol can cause immunosuppression, which results in increased risk of illness such as cardiovascular (heart) problems.
The role of stress in illness
Prolonged periods of stress can cause physical illness, such as cardiovascular disorders. A key mechanism through which this happens is immunosuppression.
Immunosuppression
Immunosuppression means a reduction in the ability of the immune system to fight off disease.
The immune system identifies foreign things like bacteria and viruses within the body and destroys them. However, cortisol reduces the production of immune cells (e.g. natural killer cells and T helper cells), which reduces the effectiveness of the immune system.
A study illustrating this is Kiecolt-Glaser et al (1984). In this natural experiment, the researchers took blood samples from 75 medical students a month before their exams and then again on the day of their exams. They found the number of natural killer cells was much lower on the day of their exams (high stress), which demonstrates a correlation between stress and immunosuppression.
In the short term, a bit of cortisol and reduced production of immune cells does not cause major problems (and actually has many benefits). However, prolonged periods of stress are associated with increased risk of diseases such as influenza and cancer. Immunosuppression is a key reason for this: There are fewer immune cells to fight off viruses and clear up cancerous cells.
Cardiovascular disorders
Cardiovascular disorders are problems of the heart.
 Stress is associated with cardiovascular disorders. For example, Yusuf et al (2004) compared lifestyle factors of 15,152 people who’d had a heart attack with a control group of 14,820 who had not had a heart attack. Based on this, the researchers identified strong correlations between stress (e.g. workplace stress and stressful life events) and heart attack.
Stress is associated with cardiovascular disorders. For example, Yusuf et al (2004) compared lifestyle factors of 15,152 people who’d had a heart attack with a control group of 14,820 who had not had a heart attack. Based on this, the researchers identified strong correlations between stress (e.g. workplace stress and stressful life events) and heart attack.
There are several ways stress can cause cardiovascular disorders. For example, stress causes blood pressure to increase and causes fat to accumulate on arterial walls. There are also more indirect mechanisms. For example, stress may increase the likelihood that a person takes up smoking, which may in turn increase the likelihood of cardiovascular problems.
AO3 evaluation points: Stress and illness
Strengths:
- Supporting evidence:
- Immunosuppression: See Kiecolt-Glaser et al (1984) above for a link between stress and immunosuppression.
- Cardiovascular disorders: As well as Yusuf et al (2004) above, the studies linking the stress-prone type A personality and cardiovascular disorders described below further support a link between stress and cardiovascular disorders.
- Practical applications: Understanding the role of stress in illness has resulted in new and better ways to prevent and treat disease. For example, ABCD.
Weaknesses:
- Conflicting evidence: Some studies suggest that certain types of stress can actually boost immunity rather than causing immunosuppression. For example, Schedlowski (1993) measured natural killer cell activity in 45 first-time parachute jumpers 2 hours before their jump, immediately after their jump, and 1 hour after their jump. The researchers found that natural killer cell activity increased immediately after the parachute jumps and then fell below baseline 1 hour post-jump. This suggests that acute (short-term) stress can initially increase immune response before resulting in immunosuppression.
- Methodological concerns: Much of the research linking stress and illness is correlational. However, as always, correlation does not necessarily mean causation. It could be, for example, that stressed people are more likely to take up smoking and that it’s the cigarettes that cause increased levels of illness rather than stress itself.
Sources of stress
Although there are many sources of stress (stressors), the A level psychology syllabus mentions 3 in particular:
Life changes
Life changes are major events that disrupt our normal ways of living. Examples of life changes that can cause stress include:
- The death of a loved one
- The birth of a child
- Moving house
- Changing job or retiring
- Getting married or divorced
Holmes and Rahe’s (1967) social readjustment ratings scale includes 43 examples of life changes and rates them according to how much stress they cause.
AO3 evaluation points: Stress caused by life changes
Strengths:
- Supporting evidence: Rahe et al (1970) got 2664 navy sailors to complete the social readjustment ratings scale prior to a 6-8 month tour of duty during which their medical records were recorded. The researchers observed a positive correlation (+0.118) between life changes (as measured by LCUs on the SRRS) and illness during the tour of duty. This supports a link between life changes, stress, and stress-related illness.
- Practical applications: Understanding the role of life changes in stress could help prevent and reduce stress-related illness. For example, a doctor could get patients to complete a self-report survey of life changes (such as the SSRS) and if the patient scores highly, the doctor could prescribe or advise treatments to manage stress.
Weaknesses:
- Other factors: Kanner et al (1981) compared the accuracy of the SRRS at predicting stress-related illness with their own hassles and uplifts scale, which is a measure of daily hassles. The researchers found the hassles and uplifts scale was a more accurate predictor of stress-related illness than the SRRS, which suggests that daily hassles are a more important cause of stress than life changes (which tend to be rare by comparison).
- Some life changes are relaxing, not stressful: The SSRS assumes all life changes are stressful, when many may actually be the exact opposite. For example, items on the SSRS include ‘vacation’ (13 LCUs) and ‘major holiday’ (12 LCUs), but many people find these life changes relaxing rather than stressful.
- Methodological concerns: A methodological concern with drawing conclusions about stress caused by life changes from the social readjustment ratings scale is that the SRRS and stress is simply correlational. As always, correlation does not necessarily mean causation and so does not prove that life changes cause stress or stress-related illness. For example, illness could be what causes life changes (e.g. time off work from being ill leads to the life change of losing a job), in which case the direction of causation is the other way round.
Daily hassles
Daily hassles are everyday irritations and annoyances, such as:
- Getting stuck in traffic
- Neighbours playing loud music
- A long queue at the supermarket
You get the idea. Kanner et al’s (1981) hassles and uplifts scale includes 117 examples of daily hassles, defined as “irritating, frustrating, distressing demands that to some degree characterise everyday transactions with the environment”.
AO3 evaluation points: Stress caused by daily hassles
Strengths:
- Supporting evidence: Kanner et al (1981) compared the ability of their hassles and uplifts scale to predict stress-related illness against the SRRS, which is a measure of stress caused by life changes. The researchers found a stronger correlation between hassles and stress-related illness than life changes and stress-related illness, which suggests that daily hassles are a more important cause of stress than life changes (which tend to be rare by comparison).
- Practical applications: Understanding the role of daily hassles in stress could help prevent and reduce stress-related illness. For example, a doctor could get patients to complete a self-report survey of daily hassles (such as the hassles and uplifts scale) and if the patient scores highly, the doctor could prescribe or advise treatments to manage stress.
Weaknesses:
- Methodological concerns: A methodological concern with drawing conclusions about stress caused by daily hassles from the hassles and uplifts scale is that even if scores are correlated with stress-related illness, this does not necessarily prove that these hassles cause stress or stress-related illness.
Workplace stress
Workplace stress comes in many forms, but the syllabus mentions 2 in particular:
- Workload: How much work a person has. If a person is given too many tasks to do within a time period, this causes stress. The higher the workload, the more stress.
- Control: The extent to which a person has influence over what work they do and how much. The less control a person has over their work, the greater the stress.
The key theory that brings these 2 factors together is Karasek’s (1979) demand-control model. According to this model, high workload increases the likelihood of stress-related illness, but this risk is reduced when the employee has more control over their work.
Other workplace stressors may include annoying colleagues and bosses, concerns about getting fired or not promoted, and even just things in the general work environment like uncomfortable chairs.
AO3 evaluation points: Workplace stress
Strengths:
- Supporting evidence: Several studies support Karasek’s (1979) demand-control model. For example:
- Workload: Kivimäki et al (2006) conducted a meta-analysis of 14 studies that included at a total of 83,104 employees and found that workload was correlated with coronary heart disease. The authors estimate that workplace stress makes employees 50% more likely to suffer from coronary heart disease.
- Control: The ‘Whitehall Studies’ conducted by Marmot et al (1997) followed 10,308 employees in the UK civil service over a period of 5 years. The researchers found that employees with low levels of control over their work were significantly more likely to suffer from heart attacks compared to employees with high levels of control over their work (even when other factors, such as diet, were controlled for).
- Practical applications: A practical application of findings from the Whitehall Studies above is that giving employees greater control over their work may reduce their risk of suffering from a heart attack.
Weaknesses:
- Conflicting evidence:
- Workload: Although the Whitehall Studies (Marmot et al (1997)) found a correlation between low levels of job control and heart disease, they found no such correlation between level of workload and heart disease. This contradicts the findings of Kivimäki et al (2006) described above and suggests higher workload does not, in fact, cause increased stress.
- Control: Meier et al (2008) tested Karasek’s (1979) demand-control model by measuring stress levels and levels of job control in 96 service employees. The researchers found that greater job control did reduce the effects of workplace stress – but only among those with an internal locus of control. For employees with an external locus of control, greater levels of job control was actually correlated with increased levels of stress-related illness.
- Methodological concerns: A methodological concern with the Whitehall Studies is that they did not control for confounding variables. The researchers focused on workload and control, but there are many other factors that may explain higher levels of stress-related illness. For example, jobs with lower levels of control may also be paid less, and these lower levels of pay may also increase the risk of stress-related illness. Such confounding variables may skew the results and decrease the validity of this study’s findings.
Measuring stress
There are several ways of measuring stress. These include self-report methods (such as the social readjustment ratings scale and the hassles and uplifts scale) and physiological methods (such as skin conductance response).
Self-report methods
Social readjustment ratings scale
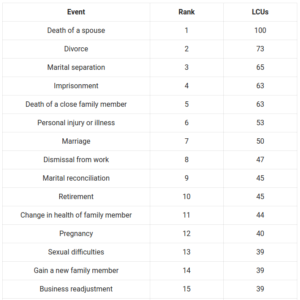 Holmes and Rahe (1967) created the social readjustment ratings scale (SRRS) to quantify the stress associated with life changes.
Holmes and Rahe (1967) created the social readjustment ratings scale (SRRS) to quantify the stress associated with life changes.
To do this, they created a list of 43 life events and asked subjects to rate how stressful each was. Based on this data, each life event was given a life change unit (LCU) score. You can see the full list here.
The more life change units a person scores on the SRRS, the greater their risk of stress-related illness:
- >300 LCUs: High risk of illness
- 150-299 LCUs: Moderate risk of illness
- <150 LCUs: Minor risk of illness
AO3 evaluation points: SRRS
Strengths of the social readjustment ratings scale:
- Supporting evidence: Rahe et al (1970) got 2664 navy sailors to complete the SRRS prior to a 6-8 month tour of duty during which their medical records were recorded. The researchers observed a positive correlation (+0.118) between life changes (as measured by LCUs on the SRRS) and illness during the tour of duty. This supports the prediction of the SRRS that LCUs would be correlated with stress-related illness, and also suggests the SRRS is a valid measure of stress.
- Practical applications: The SSRS could potentially be used to prevent stress-related illness. For example, a doctor could get patients to complete the SSRS and if the patient scores more than 300 LCUs, the doctor could prescribe or advise treatments to manage stress.
Weaknesses of the social readjustment ratings scale:
- Conflicting evidence: Kanner et al (1981) compared the ability of their hassles and uplifts scale to predict stress-related illness against the SRRS. The researchers found a stronger correlation between scores on the hassles and uplifts scale compared to the SRRS, which suggests that the hassles and uplifts scale is a more accurate measure of stress than the SRRS.
- Doesn’t distinguish between positive and negative life changes: The SSRS assumes all life changes are stressful, when many may actually be the exact opposite. For example, items on the SSRS include ‘vacation’ (13 LCUs) and ‘major holiday’ (12 LCUs), but many people find these life changes relaxing rather than stressful.
- Methodological concerns: As always, correlation does not necessarily mean causation. Even if scores on the SRRS are correlated with illness, it does not necessarily prove that life changes recorded by the SRRS caused those illnesses. For example, illness could be what causes life changes (e.g. time off work from being ill leads to the life change of losing a job), in which case the direction of causation is the other way round.
- Less scientific: As a self-report method, the SSRS relies on the participant’s subjective interpretation of events (e.g. “trouble with in-laws” is open to interpretation and may differ between people). As such, the SSRS can be said to be less scientific than physiological measures such as skin conductance response, which produce objective and quantifiable data.
Hassles and uplifts scale
Kanner et al (1981) created the hassles and uplifts scale to quantify the stress associated with daily hassles.
The hassles and uplifts scale includes 117 examples of daily hassles, as well as 135 examples of ‘uplifts’ (i.e. positive experiences). Examples include:
| Hassles | Uplifts |
| Concerns about weight | Relating well with your spouse or lover |
| Health of a family member | Relating well with friends |
| Rising prices of common goods | Completing a task |
| Home maintenance | Feeling healthy |
| Too many things to do | Getting enough sleep |
The researchers got 100 participants to complete the hassles and uplifts scale by ticking which hassles and uplifts they had encountered over the previous month each month for 9 months. They found high scores for hassles were positively correlated with stress and health problems. They also found that high scores for uplifts were negatively correlated with stress and health problems – but only among women.
AO3 evaluation points: Hassles and uplifts scale
Strengths of the hassles and uplifts scale:
- Supporting evidence: Further to the evidence above, Kanner et al (1981) compared the correlation between stress-related illness and scores on their hassles and uplifts scale with the correlation between scores on the SRRS and stress-related illness. They found a stronger correlation with stress-related illness from scores on the hassles and uplifts scale compared to the SRRS, which suggests that the hassles and uplifts scale is a more accurate measure of stress than the SRRS.
- Practical applications: The hassles and uplifts scale could potentially be used to prevent stress-related illness. For example, doctors could get patients to complete the hassles and uplifts scale and if they score highly, the doctor could prescribe or advise treatments to manage and cope with stress.
Weaknesses of the hassles and uplifts scale:
- Conflicting evidence: Although there is fairly good evidence of a link between hassles and stress-related illness, there is little research supporting a link between uplifts and reduced stress. For example, even Kanner et al (1981) above does not support a link between uplifts and reduced stress in men, only in women. Similarly, DeLongis et al (1982) gave 100 adults aged 45-64 the hassles and uplifts scale and found uplifts made little difference to stress-related illness.
- Methodological concerns:
- Retrospective: The hassles and uplifts scale is retrospective, meaning respondents must remember hassles and uplifts over a period of time (e.g. the last month). However, if a person has a bad memory, their responses may not be valid.
- Correlation does not necessarily mean causation: Even if scores on the hassles and uplifts scale are correlated with illness, it does not necessarily prove that the hassles recorded by the hassles and uplifts scale caused stress or stress-related illnesses.
- Ambiguous: Further, many of the items on the hassles and uplifts scale are open to interpretation (e.g. what one person considers “relating well with friends” another person may not) and so the results may not be valid.
- Less scientific: As a self-report method, the hassles and uplifts scale relies on the participant’s subjective interpretation of events (e.g. what counts as “relating well with friends” may differ from person to person). As such, the hassles and uplifts scale can be said to be less scientific than physiological measures of stress such as skin conductance response, which produce objective and quantifiable data.
Physiological methods
There are several physiological methods for measuring stress. For example, cortisol levels in the blood and urine can be measured, and changes in blood pressure provide a reasonable proxy for changes in stress levels. But the syllabus mentions one physiological measure of stress in particular: Skin conductance response.
Skin conductance response
Water conducts electricity. And when a person is stressed, they sweat more. So, when a person is stressed, their skin conducts electricity more easily. This is how skin conductance response measures stress.
If you’ve ever seen a lie detector/polygraph test, these work by measuring skin conductance:
- Electrodes are attached to the subject’s fingers
- These electrodes apply a tiny electrical current that enables the subject’s skin conductance to be measured
- The subject is first asked to sit still for 30 mins or so to establish a baseline (non-stressed) level of skin conductance
- The subject is asked questions
- If the subject lies when answering, this causes stress, triggering the sympathetic nervous system to increase sweat
- This increase in stress is detected as an increase in skin conductance relative to their baseline (non-stressed) level of skin conductance
AO3 evaluation points: Skin conductance response
Strengths of skin conductance response:
- Supporting evidence: Several studies have demonstrated strong correlations between levels of stress and skin conductance. For example, Harrison et al (2006) measured skin conductance in infants when they were undergoing a stressful procedure (blood sampling) and when they were undergoing a non-stressful procedure (feeding or having a nappy changed). Skin conductance increased significantly during the stressful procedure but not during the non-stressful procedure, which supports the validity of skin conductance as a physiological measure of stress. Another example is Kurniawan et al (2013), who found that trained polygraph operators were able to accurately determine (using skin conductance response) whether a person was experiencing high stress or low stress 70% of the time.
- Practical applications: Skin conductance (as measured by polygraph testing) is commonly used as a lie detector test. This can be used by law enforcement, as demonstrated in the Chris Watts police interview above, to help determine a suspect’s guilt.
- More objective and scientific: Skin conductance response uses objective and quantifiable data to measure stress. As such, it can be said to be more scientific than self-report measures of stress, which rely on a person’s subjective interpretation of events.
Weaknesses of skin conductance response:
- Conflicting evidence: Although there is lots of evidence supporting the correlation between skin conductance and stress, it is not a perfect measure. For example, even though Kurniawan et al (2013) found polygraph operators were able to accurately distinguish between high and low stress 70% of the time, this still leaves 30% of the time when they got it wrong. This demonstrates that skin conductance response is not a perfectly accurate measure of stress.
 Misuse: Although lie detection can be a useful application of skin conductance response, polygraph testing is not 100% accurate. Because of this, use of skin conductance response to determine whether someone is lying can lead to negative consequences. A potential example of this is Steve Dymond, who committed suicide after failing a polygraph test on the Jeremy Kyle talk show. Before his death, Dymond insisted he was telling the truth.
Misuse: Although lie detection can be a useful application of skin conductance response, polygraph testing is not 100% accurate. Because of this, use of skin conductance response to determine whether someone is lying can lead to negative consequences. A potential example of this is Steve Dymond, who committed suicide after failing a polygraph test on the Jeremy Kyle talk show. Before his death, Dymond insisted he was telling the truth.
Individual differences in stress
There are many nomothetic ways of psychologically classifying people, and these differences between individuals and groups of individuals may mean differences in stress levels, stress responses, and stress-related illnesses.
The individual differences in stress mentioned on the syllabus are personality types (A, B, and C) and hardiness. The syllabus also mentions gender differences in coping with stress.
Personality types
Types A and B
Friedman and Rosenman (1959) were interested in correlations between psychological personality types and cardiovascular disorders such as coronary artery disease. They identified certain patterns of behaviour, which they characterised into two personality types: Type A personality and Type B personality.
| Type A | Type B |
| Time-urgent, impatient, rushed | More patient |
| Competitive, perfectionistic | Less competitive |
| Hostile, aggressive, irritable | More calm |
For simplicity, you can think of type A as the stressed personality and type B as the non-stressed personality. The researchers found that type A personalities are associated with higher levels of stress-related illness than type B personalities:
- Type A personality types were more prone to developing heart disease
- Type B personality types were less prone to developing heart disease.
Type C
Later research (Greer and Watson (1985)) identified a further personality type: The Type C personality.
| Type C |
| Introverted |
| Neurotic |
| Represses emotions |
| Conflict-avoidant |
| People-pleaser |
Type C personalities are said to be more prone to stress than people who, for example, express their emotions freely and assert themselves. The researchers found that type C personalities are also associated with a higher risk of developing cancer. Some studies suggest this is due to immunosuppression.
AO3 evaluation points: Personality types and stress
A general point with these links between personality types and stress-related illness is that the risks are relative: Type A personalities are more likely to get heart disease than Type B personalities, but this does not mean it is likely (in absolute terms) that type A personalities will get heart disease. (Illustrative example: Someone with a 2 in a million change of getting ill, say, is twice as likely to get ill as someone with a 1 in a million chance of getting ill – but 1 in a million is still a very low chance in absolute terms!)
Strengths of personality types and individual differences in stress:
- Supporting evidence:
- Types A and B: Rosenman et al’s (1976) Western Collaborative Group Study determined the personality type (A or B) of 3,154 employed men who were not suffering from heart disease. At the follow-up 8.5 years later, 257 had developed heart disease. Type A personalities were approximately twice as likely to be among these 257 men than type B personalities, which supports a link between type A personality and heart disease.
- Type C: A review by Temoshok (1987) looked at cancer rates and personality traits associated with type C, such as a tendency to repress emotions (particularly anger). She found that these personality traits were indeed correlated with an increased risk of cancer.
Weaknesses of personality types and individual differences in stress:
- Conflicting evidence: Ragland and Brand (1988) followed up with the 257 subjects from Rosenman et al’s (1976) Western Collaborative Group Study who had suffered from heart disease. Of the 231 subjects who initially survived a heart attack, type B personalities were more likely to have died at the follow up than type A personalities. This contradicts the original findings by Roseman et al (1976) and suggests type A personalities may actually have lower risk of stress-related illness and death in some circumstances.
- Classification issues: Several researchers have argued that the general category of type A personality is too broad. For example, Matthews and Haynes (1986) and Dembroski et al (1989) found that hostility alone predicts heart disease just as accurately as type A personality does. This suggests that some components of the type A personality (such as being competitive) are not relevant to differences in stress and stress-related illness.
- Methodological concerns: Correlation vs. causation: All the studies discussed here are correlational – they look for correlations between certain personality traits and certain illnesses. But, as always, correlation does not prove causation.
Hardiness
 Kobasa (1979) identified hardiness as a factor that influences the development of stress-related illness. According to Kobasa, the hardy personality type consists of 3 key features:
Kobasa (1979) identified hardiness as a factor that influences the development of stress-related illness. According to Kobasa, the hardy personality type consists of 3 key features:
- Commitment: Hardy people are highly committed to what they do. They feel a strong sense of purpose and meaning in their life and activities – their work, their relationships, their hobbies, and so on.
- Challenge: Hardy people interpret stressors as challenges to be overcome and an opportunity to grow and improve. For example, they may seek out activities and tasks that other people find stressful, such as endurance races or difficult tasks at work.
- Control: Hardy people have an internal locus of control. This means they believe that their own choices are what shape their life rather than external factors outside of their control.
In contrast, the non-hardy personality type is the opposite of this: They give up easily (low commitment), feel unable to cope with stressors (rather than seeing them as challenges), and have an external locus of control.
Kobasa (1979) used the social readjustment ratings scale to identify 161 subjects who had undergone high levels of stress over the last 3 years. Of these 161 stressed individuals, 75 had suffered stress-related illness, whereas 86 had not. She then compared the personality traits of these two groups and found that the 86 subjects who did not get ill scored much higher for hardiness (i.e. demonstrated commitment, challenge, and control) than the 75 subjects who did get ill. This suggests that hardy personality types are more resistant to stress-related illnesses even when actual levels of stress are similar.
AO3 evaluation points: Hardiness and stress
Strengths of hardiness and individual differences in stress:
- Supporting evidence: Maddi (1987) studied 400 employees at an American phone company during a stressful time when many people were being made redundant. He observed that two-thirds (66%) of employees suffered stress-related illness during this time, but one-third (33%) did not. The one-third who did not suffer from stress-related illness were much more likely to score highly for hardiness (i.e. commitment, challenge, and control) than the two-thirds who did get ill. This supports the idea that hardiness protects against the effects of stress.
- Practical applications: Maddi (1998) hardiness training ABCD.
Weaknesses of hardiness and individual differences in stress:
- Relative importance of different components: Some studies suggest that some of the 3 C’s of hardiness – commitment, challenge, and control – are more important than others.
- Vague: The concept of hardiness is difficult to quantify objectively. Funk (1992) points out that several different scales are used to measure hardiness and that there is little research comparing these different scales. Further, it may be that what some of these scales measure is actually neuroticism – and that it is low levels of neuroticism, not hardiness, that prevents stress-related illness.
- Methodological concerns: The usual correlation vs. causation argument applies here. Even if having a hardy personality is correlated with lower levels of stress-related illness, this does not prove that having a hardy personality causes lower levels of stress-related illness. It may be, for example, that people with hardy personalities are more likely to take part in physical exercise, in which case it is likely to be the physical exercise that causes lower levels of stress-related illness.
Gender differences
Gender differences in stress may include how men and women feel stress, as well as differences in how men and women cope and respond to stress.
On average, the sympathomedullary fight or flight response differs between men and women. As discussed in the issues and debates topic, the phrase ‘fight or flight’ is an example of (beta) gender bias because it’s based solely on observations of male behavioural responses to stress. However, when Taylor et al (2000) observed the female behavioural responses to stress, they found women behaved more calmly and responded by protecting and caring for their offspring and seeking social support from friends and family. So, rather than ‘fight or flight’, the female behavioural response to stress can be characterised as ‘tend and befriend’. A potential mechanism for these differences in stress behaviours is differences in oxytocin levels.
AO3 evaluation points: Gender differences in coping with stress
Strengths of gender and individual differences in stress:
- Supporting evidence: Taylor et al’s (2000) finding – that the female response to stress is more tend and befriend and that the male response to stress is more fight or flight – has been replicated in other studies. For example, ABCD.
- Practical applications: ABCD
Weaknesses of gender and individual differences in stress:
- Conflicting evidence: ABCD.
- Questions of causal mechanisms: ABCD
- Methodological concerns: ABCD.
Managing stress
There are many ways of managing stress – these may be biological or psychological methods:
- Drugs such as benzodiazepines and beta blockers
- Stress inoculation therapy
- Biofeedback
- Social support
Drug therapy
The biological approach to managing stress is drug therapy, such as the anti-anxiety medications benzodiazepines and beta blockers.
Benzodiazepines
Benzodiazepines, such as Valium, increase the effects of a neurotransmitter called gamma-aminobutyric acid (GABA).
 GABA is an inhibitory neurotransmitter which, if you remember from the biopsychology topic, means it decreases the likelihood that the neuron will fire. By increasing the effects of GABA, benzodiazepines reduce activity in the nervous system and counteract the effects of excitatory neurotransmitters such as serotonin. This reduced activity results in increased feelings of calm and relaxation, with reduced feelings of anxiety and stress.
GABA is an inhibitory neurotransmitter which, if you remember from the biopsychology topic, means it decreases the likelihood that the neuron will fire. By increasing the effects of GABA, benzodiazepines reduce activity in the nervous system and counteract the effects of excitatory neurotransmitters such as serotonin. This reduced activity results in increased feelings of calm and relaxation, with reduced feelings of anxiety and stress.
Beta blockers
Beta blockers reduce activity of the sympathetic nervous system by blocking beta-adrenergic receptors.
As mentioned above, stressors cause the release of the hormones adrenaline and noradrenaline. When these hormones stimulate beta-adrenergic receptors in the heart and brain, it causes an increase in heart rate and blood flow. Beta blockers work by occupying these beta-adrenergic receptors – blocking them – so that adrenaline and noradrenaline can’t produce their usual effects. This reduces some of the physical symptoms of anxiety and stress, such as increased heart rate.
AO3 evaluation points: Drug therapy for stress
Strengths of drug therapy for managing stress:
- Supporting evidence:
- Benzodiazepines: ABCD.
- Beta blockers: ABCD.
Weaknesses of drug therapy for managing stress:
- Side effects: Both benzodiazepines and beta blockers produce side effects that must be weighed against the benefits of stress reduction:
- Benzodiazepines: ABCD.
- Beta blockers: ABCD.
- Addictive: Benzodiazepines are highly addictive (but beta blockers are not addictive).
- Mechanism: Drug therapy does not tackle the underlying cause of stress, but just masks the physiological symptoms.
Stress inoculation therapy
Meichenbaum (1985) describes stress inoculation therapy, which is a form of cognitive behavioural therapy.
There are 3 components to stress inoculation therapy:
- Conceptualisation: The therapist helps the patient identify and understand stressors in their life and gets the patient to think about how they ordinarily deal with them. Negative strategies for dealing with stressful situations are identified. For example, some people make their stress worse with exaggerated or unrealistically negative thinking (e.g. “I can’t cope with this work, I’m going to get fired”).
- Skill acquisition and rehearsal: The therapist teaches the patient techniques to deal with stressors more effectively. These techniques may include relaxation strategies (e.g. breathing techniques or meditation) as well as cognitive strategies, such as identifying exaggerated negative self-talk and replacing it with more realistic alternatives (e.g. “I can do this work if I take it one step at a time, I’m not going to get fired for minor mistakes”).
- Application: The therapist and patient practice using these newly-learned skills and techniques. This may just involve visualisation or role-play at first, before using them in real-life in stressful situations (with the support of the therapist).
AO3 evaluation points: Stress inoculation therapy
Strengths of stress inoculation therapy for managing stress:
- Supporting evidence: A meta-analysis by Saunders et al (1996) concluded that stress inoculation therapy was effective at reducing anxiety and improving performance under stress.
- No side effects: Unlike drug therapy, stress inoculation therapy does not have a risk of side effects.
Weaknesses of stress inoculation therapy for managing stress:
- Individual differences: Stress inoculation therapy is time-consuming and takes a lot of effort on behalf of the patient. As such, many patients may quit without seeing results.
- Cost and difficulty: ABCD
Biofeedback
 Biofeedback teaches people to identify and control the physiological processes of stress, such as elevated heart rate and muscle tension. This results in positive feelings of relaxation and reduced stress that reinforce these stress-controlling behaviours via the principle of operant conditioning:
Biofeedback teaches people to identify and control the physiological processes of stress, such as elevated heart rate and muscle tension. This results in positive feelings of relaxation and reduced stress that reinforce these stress-controlling behaviours via the principle of operant conditioning:
- Awareness: First, the person needs to be aware when they’re experiencing the physiological symptoms of stress. Machines such as heart rate and blood pressure monitors, or skin conductance polygraph machines, can all be used to provide feedback to the person (e.g. in the form of a visual display on a screen) that they’re experiencing a physiological stress response.
- Control: Next, the person is taught techniques to control these physiological symptoms when they occur, such as meditation or breathing techniques. The person practices these techniques whilst paying attention to feedback from the machine (e.g. looking at their heart rate on a heart rate monitor) to try and reduce this physiological response (e.g. trying to make heart rate go down).
- Positive reinforcement: Feedback from the machine can act like a sort of game, providing positive reinforcement of effective stress-reduction techniques. The increased feelings of relaxation also positively reinforce the stress-reduction techniques.
- Application: Finally, when the person is able to control their physiological stress response, they apply the techniques they’ve learned in biofeedback to real-life stressful situations.
AO3 evaluation points: Biofeedback
Strengths of biofeedback for managing stress:
- Supporting evidence: A randomised controlled trial by Lemaire et al (2011) found biofeedback resulted in significant and lasting stress reductions (as measured by self-report questionnaire) that were not observed in the control group.
- No side effects: Unlike drug therapy, biofeedback does not have a risk of side effects.
Weaknesses of biofeedback for managing stress:
- Conflicting evidence: Greenhalgh et al (2010) reviewed randomised controlled trials of biofeedback for reducing high blood pressure (an objective measure), but found no difference in results between biofeedback and placebo. This could suggest biofeedback only reduces feelings of stress (e.g. as measured by self-report measures like in Lemaire et al (2011) described above) without actually reducing the risk of stress-related illness.
- Cost and difficulty: Biofeedback can be expensive and may not work for all patients.
Social support
Social support – i.e. support from friends, family, colleagues, etc. – helps people deal with stress and lessen the effects of stressors.
There are several different forms social support can take:
- Instrumental support: Practical help. For example, if a friend is stressed out because they can’t pay their bills, instrumental support might involve giving them some money. If a family member is stressed out by a house renovation, instrumental support might involve plastering the walls or doing some plumbing for them. This reduces stress by tackling the stressor.
- Emotional support: Helping improve someone’s mood by providing care and comfort. For example, if a friend is stressed out by relationship problems, emotional support may involve listening to them and empathising with their situation. This reduces stress by counteracting the negative emotions (and physiological mechanisms) of stress.
- Esteem support: Helping improve someone’s confidence in their ability to deal with a stressor. For example, if a colleague is stressed out by a difficult work assignment, esteem support may involve telling them how skilled they are and reminding them of past successes. This reduces stress by increasing the person’s belief that they are able to cope with the stressor and overcome the challenge.
AO3 evaluation points: Social support in coping with stress
Strengths of social support for managing stress:
- Supporting evidence: Orth-Gomér et al (1993) conducted a 6-year longitudinal study of 736 Swedish men aged 50. The researchers found smoking and lack of social support were the 2 factors most strongly correlated with heart disease during the period of the study, which supports the idea that social support is effective at managing stress and reducing stress-related illness.
Weaknesses of social support for managing stress:
- Methodological concerns: As always, correlation (e.g. as demonstrated in Orth-Gomér et al (1993) above) does not prove causation. It’s not clear how social support may reduce stress or stress-related illness.
- Individual differences: Not all social support may be helpful. For example, instrumental support in the form of financial gifts may make a person feel guilty, increasing stress rather than decreasing it. Or, if a person has friends who deal with stress by turning to alcohol or drugs, social support could be counterproductive rather than helpful.
<<<Relationships
or:
<<<Gender
or:
<<<Cognition and development
Aggression>>>
or:
Forensic psychology>>>
or: